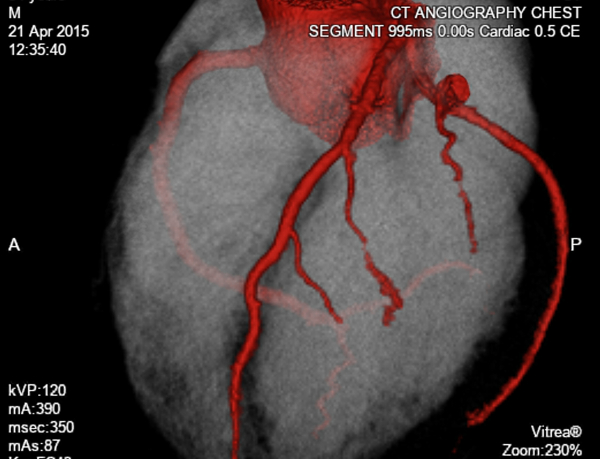
CT coronary angiography (CTCA) is a non invasive test for assessment of coronary arteries to exclude coronary artery disease (CAD). It involves administration of intravenous contrast, and imaging the heart with multi slice computed tomography (CT). This is done over multiple heart beats, in the same part of the cardiac cycle (with help of ECG gating). This data is then assembled to review the coronary arteries in multiple planes.
Clinical assessment prior to the scan by the referring physician is important in selecting suitable candidates for the test.
This includes:
- Patient ability to follow simple instructions
- Normal renal function
- Not currently pregnant
- Able to lie flat
- Able to hold a breath for 10 seconds
- No contraindications to beta blockers or calcium antagonists.
If the patient's heart rate is more than 60 beats per minute, two 50 mg oral doses of metoprolol are prescribed, one the night before and one on the morning of the test. Supplementary oral and intravenous beta blockers may be required immediately before the scan. Sublingual glyceryl trinitrate is also administered during the scan to dilate the coronary arteries. A heart rate of 60 bpm or less is ideal for the test, as with even small increases in heart rate, image quality drops perceptibly.
The Cardiac Society of Australia and New Zealand (CSANZ) recommends that the test is most appropriate for patients with a low or intermediate pre test probability of CAD, who otherwise would have been considered for invasive coronary angiography. (The latter carries some risks such as bleeding.) Approximately 15% of invasive coronary angiograms are normal and substituting these with a non invasive test would be beneficial.
Recent advances in CT techniques have resulted in significant reduction in radiation exposure from the test. The most important of these are prospective ECG gated scanning and tube modulation. This means that X-rays are only used during the relevant phase (usually late diastole) of the cardiac cycle. In the remainder of the cardiac cycle there is no radiation exposure. The lowest possible tube current also helps reduce the radiation dose.
The average background yearly radiation exposure is approximately 3 mSV (milli Sieverts). As a comparison, a traditional invasive diagnostic angiogram has an average radiation of 7 - 8 mSv (higher doses likely if patient proceeds to angioplasty or stent insertion). Depending on patient size and heart rate, CTCA radiation doses vary between 3 - 6 mSv.
Meta-analyses of more than 45 clinical trials has concluded that CTCA's ability to diagnose significant disease (defined as stenosis of more than 50%) is excellent, when compared with invasive coronary angiography. CTCA has a high negative predictive value (NPV) of 96 - 100%, and a positive predictive value (PPV) of 93%.
As such, it is recommended as a tool for ruling out significant CAD in patients with stable symptoms with a low or intermediate probability of CAD.
CSANZ recommends reporting of stenoses in broad categories, rather than numeric stensoses, due to lower resolution than invasive angiography at present. These include:
- Normal 0%
- Minimal <25% stenosis - Medical management
- Mild 25 - 49% - Medical management
- Moderate 50 - 69% - Further assessment (possibly a cardiac stress stress to assess the significance of the stenosis, or invasive angiography)
- Severe >70% - Further assessment
In addition to the above, the following indications are considered appropriate for CTCA by CSANZ:
- Investigation of equivocal or uninterpretable cardiac stress test
- Evaluation of new onset heart failure or cardiomyopathy of unknown aetiology
- Evaluation of left bundle branch block
- Mapping of coronary vasculature including internal mammary arteries before repeat bypass graft surgery
- Excluding significant CAD before non coronary cardiac surgery
- Evaluation of suspected coronary anomalies and complex congenital heart disease