Dr Andrea Zarkovic shares valuable tips on maintaining vision in AMD patients in the primary care setting.
Patients with age-related macular degeneration (AMD) and those at high risk of developing the disease make up a large proportion of patients attending general practice.GPs can play an important role in the diagnosis and management of patients with macular degeneration.
Who should be checked for wet AMD?
Prevalence of AMD-related blindness in Australia has declined in recent years. While this is largely due to successful treatment, the key to success has been early diagnosis prompted by awareness of AMD in the general population and medical community.
The recent National Eye Health Survey showed AMD is found in more than 25% of Australians over the age of 50. While the majority will have a mild form of AMD, the risk of vision-threatening late stage AMD increases exponentially with age: 7% prevalence of late AMD is found in those over 80 years.1 Therefore, even asymptomatic patients over the age of 60 years should be encouraged to see an eye specialist on a regular basis, at least every few years.
Early detection is the one of the most important prognostic factors for wet age-related macular degeneration (wAMD). Any symptoms of distortion, sudden or rapid onset of blurry vision or dark patches in a patient’s central vision could signify development of choroidal neovascularization and should prompt urgent referral to an Ophthalmologist. Patients whose wAMD is picked up early, i.e. before significant visual loss occurs, have a much better response to treatment and a better long term prognosis.
AMD is found in more than 25% of Australians over the age of 50 [but] the prevalence of AMD-related blindness has declined.
At least 70% of AMD cases have a genetic link, with 50% of patients whose first-degree relative is affected can be expected to develop AMD. Therefore, it is crucial to advise parents, siblings and children of those affected by AMD to get their eyes tested at regular intervals.
Risk factors
Smoking is the most important modifiable risk factor for AMD and is directly linked to vascular inflammation and endothelial damage found in neovascular AMD. Smokers have a four-fold increased risk of development of AMD compared to non-smokers and the onset of their disease tends to be much earlier. In addition, some studies have found that smokers have a poorer response to therapy than non-smokers. Smokers with a diagnosis of wAMD or those with a genetic predisposition need to be made aware of the importance of quitting and supported in their efforts as much as possible. Obesity and high cholesterol may also increase the risk of AMD and there may need to be a lower threshold for treatment in predisposed individuals.
Diet and vitamin supplements
The role of diet and vitamin supplements in AMD has been extensively studied. A healthy diet high in antioxidants, green leafy vegetables and Omega 3 is beneficial for good macular health. Those with inadequate dietary vitamin intake and patients with moderate macular degeneration or late macular degeneration in one eye can potentially reduce their risk of AMD progression by 20% with the use of specific dietary supplements.
The recommended supplements are formulated according to the Age-Related Eye Disease Study 2 (AREDS 2) formula and contain vitamins C and E, zinc, copper, lutein and zeaxanthin. Beta-carotene has been removed from the formula due to increased risk of lung cancer in smokers. Ophthalmologists usually advise patients who are considering vitamin supplements to check with their GP to ensure that the supplements will not interact with other medicines or supplements.
Diagnosis
Asymptomatic patients should have their macula checked as part of their routine eye health check with their optometrist. Symptomatic patients should be referred straight to an Ophthalmologist in order to ensure prompt diagnosis and minimal inconvenience to the patient.
Diagnostic tools used by Ophthalmologists to diagnose and monitor wAMD include ocular coherence tomography (OCT), fluorescein angiography (FFA) and OCT angiography (OCTA). OCTA is the latest advance in retinal imaging and because it is non-invasive, is particularly useful in patients with poor venous access, allergy to fluorescein or the frail elderly.
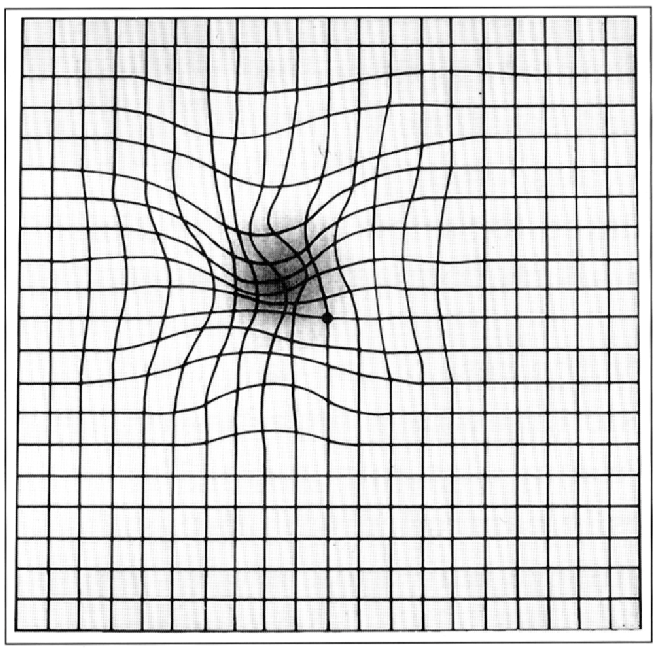
Patients with AMD and those at high risk of developing the disease should use an Amsler grid for self-monitoring at home. The Amsler grid was first described in 1947 by Marc Amsler, this chart consists of a 10 cm square with a grid and a central spot for fixation.
Treatment
The mainstay of treatment of wAMD is intravitreal anti-VEGF injections. There are two anti-VEGF drugs, Lucentis and Eylea that are PBS listed and readily available. The injections are usually given as an induction of monthly treatments for three months and the treatment is then tailored according to the response. The treatment is given either in the sterile environment of a day surgery setting, in which case the cost is often covered by the health fund, or in the clinic rooms. The patients can be reassured that the eye will be numb and the injection is often less uncomfortable than having a blood test.
Ophthalmologists usually advise patients who are considering vitamin supplements to check with their GP to ensure these will not interact with other medicines or supplements.
If a patient has had a recent stroke, a heart attack or any infections, the Ophthalmologist needs to be informed as this will influence the timing of the anti-VEGF treatment.
Support for AMD patients
GPs, Ophthalmologists and optometrists provide a vital support structure for patients with declining vision. Ophthalmologists refer patients to providers of low vision aids such as Vision Australia and Quantum Vision while GPs can help with extra support in the community such as home help and transport. It is important that patients with AMD have regular checks with their eye specialist to ensure their glasses are as up to date as possible to maximize their vision. Macular Disease Foundation Australia provides information and support for people with macular conditions.
*Dr Andrea Zarkovic MBChB, PGDipOphthBS is an Ophthalmologist with myEyeSpecialist, Ballina and Robina.