
Aussie Docs share a common goal
The Docceroos are a group of medical practitioners who literally share a common goal – we are all passionate football enthusiasts. While each specialises in different practice fields and hails from various parts of Australia, our love for not just watching the “round ball game” but playing it, has taken us around the globe.
Every year, we assemble a team to compete in the annual World Medical Football Championships (WMFC), held in a foreign country. Our journey began in 2003 when Dr. Alan Jones swiftly assembled a squad of 14 players in just six weeks to participate in Barcelona, at the prestigious Football Estadi venue and the training fields of F.C. Barcelona.
- Details
- Written by: Jason Koutadontis, Docceroos goalkeeper

After the Rain, the restoration
It is now 18 months since our Lismore medical practice was inundated by the floods. In some ways it feels like an eternity but in others it feels quite recent, as we are still dealing with the fallout and impacts, not just on our practice but also within the community.
The flood has changed our practice profoundly and permanently. Fortunately, at this distance from the event, there seem to be as many positive aspects to the change as negative ones.
Financially we are still challenged, but no longer facing bankruptcy. We have taken steps to “insure” ourselves as we can no longer get even a quote for flood insurance. Some 18 months on, we are not yet done with the repairs to the property but we are down to the less important repairs, such as fixing the potholes in the driveway (quote - $38,000.00).
- Details
- Written by: Dr Nina Robertson

Just a minute…
A quick chat with Tracey Maisey, New Chief Executive, Northern NSW Local Health District
Q: What do you see as the significant opportunities facing this regional health service?
A: One of the significant opportunities for the NNSWLHD is continuing to strengthen our exceptional health workforce. We have a growing population, a beautiful climate, and a wonderful health service, so we’re working to capitalise on these things to future-proof our local workforce.
We’re focused on ensuring equity of access to health services for our communities, in particular Aboriginal and Torres Strait Islander people, and people who require mental health, alcohol and other drugs services.
Our populations are spread over a large geographical area, so ensuring people in all reaches of NNSWLHD have the right access to services is something that I’m focussed on.
Integration with local General Practices is extremely important, and I look forward to working closely with primary health partners in the area.
Finally, I want to strengthen our connection with our communities to ensure they have an active voice in our services.
Q: Have you encountered any major surprises since starting in the job?
- Details
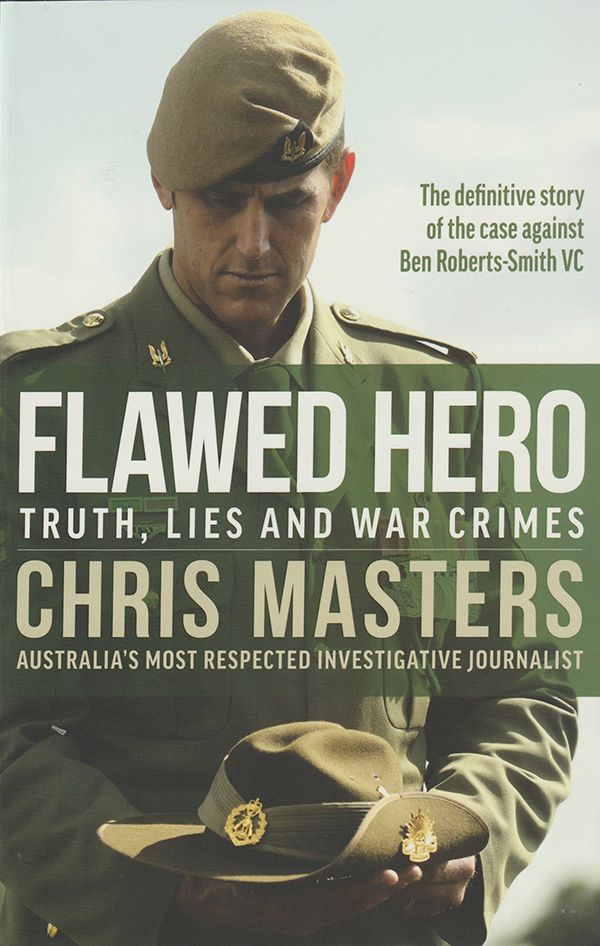
Book Review - Flawed Hero Truth, Lies and War Crimes
Flawed Hero Truth, Lies and War Crimes
by Chris Masters, Allen &Unwin 566pp
Not long into this hefty account it becomes clear that the title is remarkably generous. Ben Roberts-Smith VC, MG was not so much a “flawed hero”, although he was certainly that, but, in the words of one of his comrades in arms, ‘an infant who ends up believing his own fantasies’, ‘a showboating piece of shit’, ‘a big boofhead’.
In more poetic words, Chris Masters, whose work includes books based on officially-approved embedding with the military in Afghanistan, calls him a “counterfeit exemplar” whose elevation to hero status did nobody, including the man himself, any favours.
Many of the other Special Air Service Regiment (SASR) personnel who served with or, often to their regret, under Roberts-Smith were similarly disparaging, not least those who were bullied by the 2.02 m (6’6”) “Big Ben”, or worse, punched by him for alleged operational shortcomings.
As unlikeable as he appears, there is no doubt that BRS, as he is known, was a good soldier, ‘good’ in the sense of battling, and most often killing, what he called the “bad cunts” who inhabited the Taliban infested parts of Afghanistan where Australian troops were deployed. BRS won the Victoria Cross for bravery, later questioned, for his engagement in a battle in 2010.
- Details
- Written by: Robin Osborne
Read more: Book Review - Flawed Hero Truth, Lies and War Crimes
Education benefits late-life work
Research studies tend to confirm what we already know, or have suspected, and such is the case with a major Australian study finding that today’s older people (50+) who left school before year 12 often struggle to work later into their lives because of poorer health, or because their work is not suitable for older personnel. Women are disproportionately impacted.
Data from the 17,000 respondents that participated in the Household Income and Labour Dynamics in Australia survey was analysed in accordance with life expectancy and quality over four periods: years working in good health, years working in poor health, years retired in good health and years retired in poor health.
- Details
- Written by: Robin Osborne
Page 5 of 177




